Side effects make or break diabetes meds for a lot of us. My dad once switched his pill, only to spend the next week battling stomach troubles. When you’re already dealing with blood sugar swings, the last thing you want is more stuff to worry about.
If you’re like my cousin who was recently diagnosed, you’ve probably heard a million names—metformin, Ozempic, Jardiance—and felt totally lost. Which really keeps your glucose in check without turning your stomach to knots or sending you running to the bathroom every hour?
Since type 2 diabetes is everywhere these days (believe me, I have more than one friend fighting it), finding meds with fewer side effects is a real priority. And while there’s no magic bullet, some medications have a solid track record for being both safe and effective. I’ll lay out the facts—what the research shows, what patients deal with in real life, and some clever tips for getting the benefits with as little hassle as possible.
- Why Side Effects Matter Most
- Metformin: The Old Reliable
- The Rise of GLP-1 Receptor Agonists
- SGLT2 Inhibitors and Their Surprises
- Practical Tips for Safer Diabetes Treatment
Why Side Effects Matter Most
No one wants to trade high blood sugar for a bunch of new problems. That’s why picking the best diabetes medication isn’t just about what drops your numbers fastest—it’s about what lets you keep living your life, too. Let’s be real: if your medicine is making you feel lousy, skipping doses or ditching it altogether gets tempting fast, and that’s when real trouble starts.
Doctors and researchers agree: side effects are the biggest reason people stop taking diabetes meds. In fact, a research review from 2023 found about one in five people with type 2 diabetes will stop or switch their medicine in the first year mainly because of how their body reacts to it. Sometimes it’s tummy issues, sometimes it’s headaches or weird swelling, or occasional allergic reactions.
Here’s why side effects are such a big deal:
- If you can’t tolerate a drug, your blood sugar can spiral out of control.
- Bad side effects can mess with your sleep, appetite, even your mood.
- Missing doses because you feel sick actually puts you at more risk of serious issues like nerve damage or kidney failure.
Different meds come with their own headaches. Some might give you diarrhea, some can make you pee more, and a few can make you gain weight or even lose too much. People often get confused because what’s mild for one person can be unbearable for someone else.
Check out this quick comparison of some common diabetes drug side effects based on recent studies:
| Medication Type | Most Common Side Effect | How Often (%) |
|---|---|---|
| Metformin | Stomach upset | 10–25% |
| SGLT2 Inhibitors (like Jardiance) | Frequent urination | 5–10% |
| GLP-1 Agonists (like Ozempic) | Nausea | 15–20% |
| Sulfonylureas | Low blood sugar (hypoglycemia) | Up to 30% |
The stats show that while side effects aren’t guaranteed, they’re definitely not rare. That’s why when you and your doctor talk meds, side effects shouldn’t be an afterthought—they need to be right up front.
Metformin: The Old Reliable
Ask any doctor about diabetes medication, and metformin nearly always tops the list. It’s been around for over 60 years, so there’s a ton of research and real-world experience behind it. Most folks starting out with type 2 diabetes will try metformin first—and for good reason.
The main way it works is by helping your body use insulin better and lowering how much sugar your liver makes. It’s not a secret weapon, but for many, it gets the job done. Plus, unlike a lot of other meds, metformin doesn’t usually cause weight gain and has a super low risk of making your blood sugar drop too low (which can be scary).
Let’s talk side effects, though. The biggest complaint? Stomach stuff—mainly nausea, loose stools, or just feeling a bit off in the gut. But here’s the thing: the stomach issues often get better after a few weeks. If not, doctors can switch you to an “extended-release” version that’s easier on your system. My buddy tried the regular tablets at first, hated it, then switched to the smoother version and said it made a world of difference.
- Doesn’t cause weight gain
- Won’t usually cause dangerously low blood sugar by itself
- Can sometimes cause B12 deficiency with long-term use (so a simple blood test checks for this every year or two)
- Rare side effect: lactic acidosis, but extremely uncommon if you have healthy kidneys
Doctors almost always recommend starting with a small dose and slowly ramping up—this helps dodge most tummy problems. Taking metformin with food (never on an empty stomach) is another solid trick. And if you ever need to take a break for medical tests with dye (like a CT scan), make sure to pause the metformin—just let your doctor guide you.
For folks looking for safe, tried-and-true options, metformin delivers for most people—without turning daily life upside down.

The Rise of GLP-1 Receptor Agonists
It’s hard to miss the hype around drugs like Ozempic, Wegovy, and Trulicity. These are called GLP-1 receptor agonists. They basically copy a hormone in your body that helps control blood sugar and keeps you feeling full longer. These meds aren’t just changing diabetes care—they’ve become kind of famous for helping with weight loss too.
Doctors like these medications because they don’t cause low blood sugar (hypoglycemia) as often as some older drugs. Honestly, that’s a big deal—low blood sugar gets scary fast. People on GLP-1s also tend to lose some weight, which is a win for a lot of folks with type 2 diabetes.
But nothing’s perfect. The most common side effects are stomach stuff—nausea, vomiting, and sometimes mild diarrhea. Usually, these issues show up in the first weeks but often calm down as your body adjusts. One thing that seems to help is starting with a low dose and letting your doctor slowly bump it up. This is called "titration," and it makes life a whole lot easier.
- GLP-1s work for both diabetes and weight loss, but their main job is to keep blood sugar steady.
- They rarely cause dangerously low blood sugar because they work only when your blood sugar is high.
- Most people see some weight loss, since these drugs help you feel fuller and eat less.
- Starting on a very low dose makes side effects way easier to deal with—tell your doctor if you’re struggling.
- People with a family history of certain thyroid problems shouldn’t use these drugs. Always check with your doctor first.
Insurance sometimes makes things tricky—these meds are not always cheap. But for those who can get them covered, GLP-1 agonists are rewriting the rules on diabetes medication that’s effective and easier to live with.
SGLT2 Inhibitors and Their Surprises
If you haven’t heard of SGLT2 inhibitors, you’re not alone—most people don’t know these drugs even exist until their doctor mentions them. The main names you’ll spot are Jardiance, Farxiga, and Invokana. What makes them different? Well, they help your kidneys flush out extra sugar through urine. It’s a pretty neat trick compared to older meds that just mess with insulin.
So, do SGLT2 inhibitors actually work? Yeah, and not just for blood sugar. Research shows they also help lower your risk for heart failure and kidney problems. That’s huge, since if your blood sugar’s off, your heart and kidneys are almost always at risk too. Some studies have even shown a 30-35% drop in hospitalization for heart failure among people taking these meds.
| Medication | Main Benefit | Common Side Effect |
|---|---|---|
| Jardiance (empagliflozin) | Protects heart, lowers A1C | Urinary tract infections |
| Farxiga (dapagliflozin) | Kidney protection, weight loss | Yeast infections |
| Invokana (canagliflozin) | Heart benefits, lowers blood pressure | Increased urination |
Now, here’s the catch—pee. Because these drugs work by making you go more often, folks notice frequent bathroom trips. My friend Sameer joked that he mapped every public restroom near his office after starting on Farxiga. Not exactly fun, but not dangerous if you stay hydrated. Another thing to watch for is yeast and urinary tract infections, especially for women. You cut your risk by keeping super clean and drinking water throughout the day.
SGLT2 inhibitors are usually added for people struggling to get their levels down with diabetes medication like metformin alone, or for those with heart or kidney issues. Most folks tolerate them pretty well, but there’s a rare, odd risk called ketoacidosis—a type of acid spike even if your sugars aren’t super high. This is rare, but if you get sick, stop eating, or feel super tired and confused, talk to your doctor right away.
- If you have low blood pressure, check with your doctor—these drugs can drop it lower.
- Always tell your doc if you’re having surgery or get a serious infection while on these meds.
- Watch for any unusual pain, dizziness, or weird-smelling breath—these could all be early warning signs for rare side effects.
For a lot of folks (especially those worried about heart problems), SGLT2 inhibitors are kind of a game-changer. Just make sure you know what to look out for so you’re not surprised along the way.

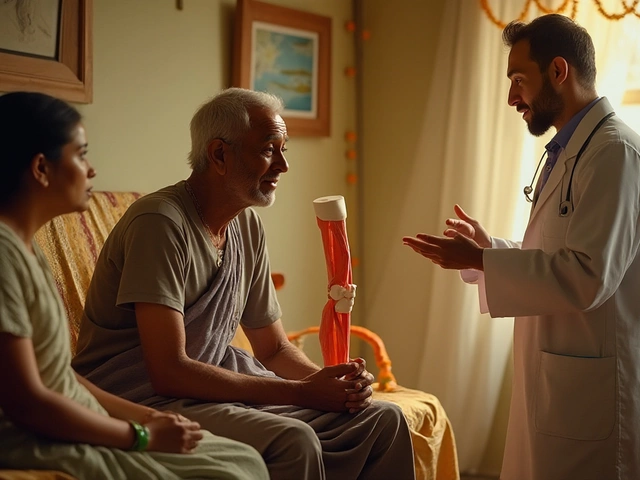
Practical Tips for Safer Diabetes Treatment
If you want fewer side effects from your diabetes medication, a little planning can go a long way. I’ve seen it in my own family—my sister-in-law switched her routine and her stomach problems practically vanished. Here’s what actually helps:
- Take meds with food. This seems basic, but it’s a real game-changer, especially with metformin. A decent-sized snack can make those nasty stomach cramps way less likely.
- Go slow with dose increases. If your doctor says it’s okay, ask about starting low and increasing gradually. One study showed that people who took more time ramping up their metformin dose had almost 40% fewer digestive issues.
- Drink plenty of water. This is especially true for SGLT2 inhibitors like Jardiance, which can dehydrate you fast. Hydration keeps headaches, dry mouth, and dizziness in check.
- Know your body’s cues. Don’t wait until you feel awful. Things like nausea, itching, or even weird muscle cramps deserve attention early. Call your doctor before things get ugly.
- Ask about extended-release options. Some meds (like extended-release metformin) cause fewer side effects than the regular types. It’s worth bringing up at your next appointment.
Everyone’s different, so don’t compare yourself too much to others at your clinic or in your family. My daughter, Avni, actually made me a sticky note for my pills: “Dad, remember your body is YOU.” She’s right—what bugs me may not bug you.
Here’s a quick look at how often people get side effects with the most common diabetes drugs:
| Medication | Common Side Effects | Percent Affected |
|---|---|---|
| Metformin | Stomach upset | 10-25% |
| GLP-1 agonists (Ozempic, Trulicity) | Nausea, diarrhea | ~20% |
| SGLT2 inhibitors (Jardiance, Farxiga) | Urinary infections, dehydration | 5-10% |
| Sulfonylureas | Low blood sugar | 10-20% |
If something feels off, don’t wait for your next appointment. Pharmacies usually have a helpline, and your doctor may have a nurse line for quick questions. Always double-check before mixing in over-the-counter meds, too—some cold pills can mess with blood sugar or interact with diabetes drugs.
The best way to get safer results is to stay honest with your healthcare team about how meds make you feel. If you’re having trouble, most doctors would actually rather know right away than get surprised by a problem later.



Rohan Talvani
I am a manufacturing expert with over 15 years of experience in streamlining production processes and enhancing operational efficiency. My work often takes me into the technical nitty-gritty of production, but I have a keen interest in writing about medicine in India—an intersection of tradition and modern practices that captivates me. I strive to incorporate innovative approaches in everything I do, whether in my professional role or as an author. My passion for writing about health topics stems from a strong belief in knowledge sharing and its potential to bring about positive changes.
view all postsWrite a comment