Imagine being so tough that you handle the word “cancer” with grit—yet, the treatments break you in ways no diagnosis ever could. Cancer alone is a nightmare, but ask anyone in the thick of chemotherapy, radiation, or a bone marrow transplant about their true horror stories. The shocking part? It’s not always the cancer that causes the worst agony. The most painful cancer treatment is a battleground of side effects, both physical and emotional, that tests every ounce of strength you’ve got. Let’s pull back the curtain on what these treatments feel like, how pain varies from one person to the next, and what actually makes some therapies stand out as the toughest.
What Makes Cancer Treatments So Painful?
Cancer treatment pain isn’t just about the intensity; it’s about how unpredictable and all-consuming it can be. Different therapies attack cancer in unique ways, leaving behind distinctive trails of misery. Chemotherapy, famous for its relentless side effects, damages fast-growing cells—including healthy ones. That means nausea that doesn’t quit, mouth sores so severe that eating is a struggle, and nerve damage that can turn a simple touch into agony. In 2022, a survey in the Journal of Pain and Symptom Management found that almost 70% of patients receiving chemotherapy reported moderate to severe pain, yet many didn’t anticipate just how much it could control their lives.
Radiation, on the other hand, can seriously burn the skin from the inside out. People compare the aftermath to severe sunburn or even second-degree burns. This suffering can last weeks, leaving people unable to wear clothing or move comfortably. The shocker? For some head and neck cancer patients, swallowing is so excruciating that they describe the pain as ‘glass shards going down.’ Here’s a quick look at some common cancer treatments and their main pain triggers:
| Treatment Type | Main Pain Triggers |
|---|---|
| Chemotherapy | Nerve pain, mouth sores, digestive pain, joint pain |
| Radiation | Severe burns, mouth/throat pain, tissue damage |
| Surgery | Incision pain, recovery complications, internal scarring |
| Immunotherapy | Bodywide aches, inflammation, autoimmune symptoms |
| Bone Marrow Transplant | Bone pain, infection, graft-versus-host disease |
Surgery pain often gets overlooked unless you’ve actually lived through it. Deep excisions to remove tumors can leave long-lasting pain, nerve damage, and scarring—especially if nerves or muscles are cut or relocated. Major cancer surgeries (think: mastectomy, esophagectomy, or limb removal) can hurt long after the wound has closed. I once sat beside my friend as she tried to lift her cup after breast surgery, stunned at how even a tiny movement sent a stab through her side.
Then you have immunotherapies and new precision drugs. Sounds gentler, right? Surprise: These can trigger the immune system so fiercely that your body attacks itself—leading to severe joint pain, skin rashes, or even trouble breathing.

The Pain Olympics: Chemotherapy, Radiation, and Bone Marrow Transplants
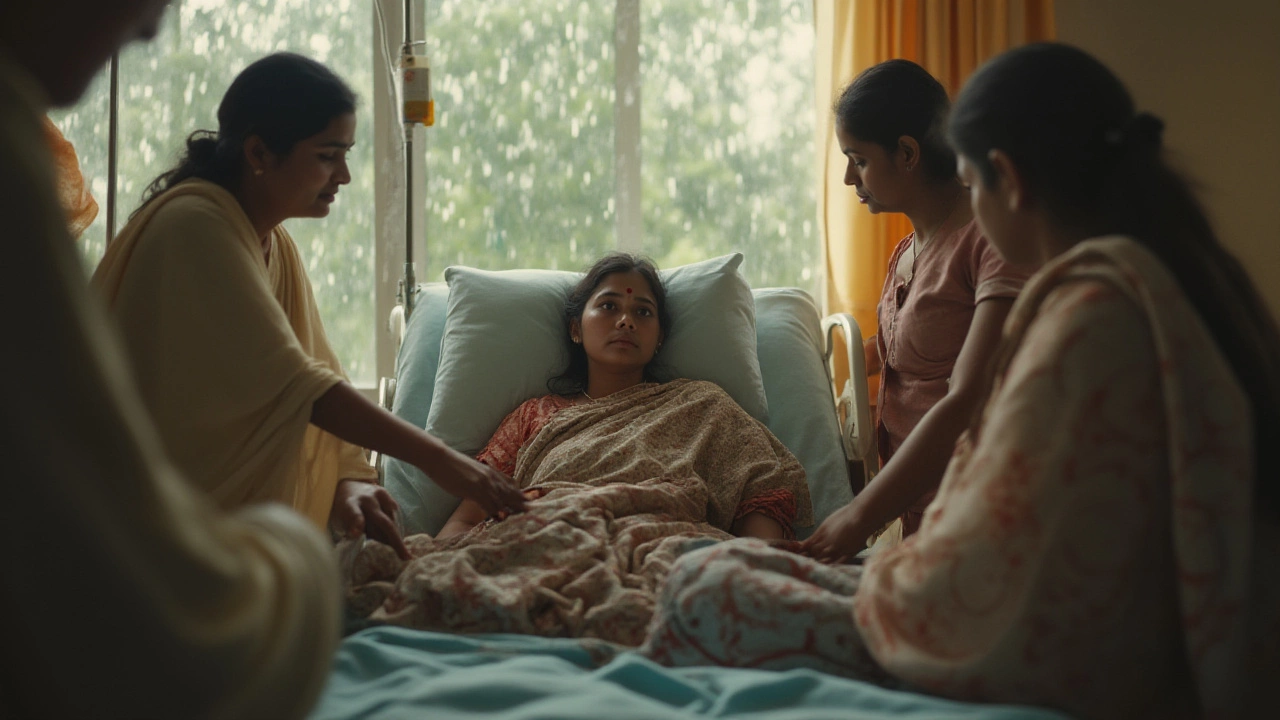
If there was a prize for the most painful cancer treatment, three contenders would battle for it: chemotherapy, radiation therapy, and bone marrow transplant. Each one is notorious, but for very different reasons, and which comes out on top depends a lot on the patient’s specific cancer and personal biology. My wife, Anjali, used to say the anticipation—the day before a chemo cycle—hurt almost as much as the nausea that followed. Psychological pain can shadow the physical, making it all worse.
Most painful cancer treatment: Let’s talk about chemotherapy first. Drug regimens like cisplatin, doxorubicin, and paclitaxel aren’t just hard on cancer—they’re hard on every cell they touch. Neutropenia (a crash in white blood cells), severe nausea, total exhaustion, and even loss of taste. And for a cruel bonus, ‘chemo-induced peripheral neuropathy’—which basically turns your hands and feet into vibrating, burning, stabbing reminders of your ordeal. Some patients compare walking to “stepping on needles with every step.” Just to put it into perspective: nearly half of all people who get certain chemo drugs develop chronic nerve pain. That’s a lot. And doctors sometimes have to reduce the dose, even if the cancer isn’t responding, just so the pain doesn’t take over their lives.
Now, radiation. It seems like a beam of light—harmless on the surface. Except it fries healthy tissue along the way. If you’re getting it for cancers in the head or neck, the mouth and throat can be devastated. Ever tried to eat with painful mouth ulcers? Imagine that, multiplied. Many folks drop serious weight, not for lack of appetite, but because swallowing just isn’t worth the pain. For pelvic cancers, radiation can scorch the intestines and bladder, leaving bathroom trips excruciating. Skin in the treatment area can peel, crack, or become raw—sometimes even months later.
And then comes the bone marrow transplant. This treatment is especially brutal because, before the new marrow can take hold, doctors wipe out your existing immune system using high-dose chemotherapy and radiation. What follows? Months of isolation, largely spent fearing infection, all while your bones ache, your gut rebels, and the skin can erupt in rashes. Worst-case scenario: graft-versus-host disease, where the new immune system simply refuses to play nice and attacks organs, joints, and skin. The pain here is deep—sometimes unresponsive to even the strongest painkillers. The emotional toll, from being cut off from loved ones during recovery, cranks up the volume on every ache.
The pain Olympics aren’t always consistent: One patient may breeze through chemo but be floored by radiation, and vice versa. Genetics, nutrition, emotional resilience, and strong support systems can shift the scales—though not always as much as one would hope. When things get unbearable, some people seek out alternative therapies. Acupuncture, physical therapy, relaxation techniques—these can help, but rarely make the pain disappear altogether.
There’s also a push toward “pain management teams” at cancer centers now. Doctors, nurses, psychologists, and rehab specialists get together and build a game plan tailored for each person. It’s not about being brave and powering through—it’s about treating pain like the enemy. Still, pain medication doesn’t always touch the worst kinds of suffering, especially nerve pain. This is where new research is heading, trying to find ways to block pain where it starts, rather than just dulling it with narcotics.
Not everything is misery, though. Advances in pain management—like nerve blocks, careful drug mixing, and even non-drug options—let some people keep their pain in check. A decade ago, most patients just had to endure; today, expectations are shifting toward a life with less suffering, even during rough treatments.

Managing Pain and Navigating the Journey: Tips and Facts
Epic pain stories grab attention, but here’s the reality: the goal now is not just to fight cancer, but to control pain so life, as messy as it gets, stays livable. No strategy covers everyone, but some ideas come up again and again among survivors, doctors, and caregivers.
First, don’t downplay pain. Telling your doctor about every twinge or torment isn’t complaining—it’s survival. Pain specialists can switch up medications, recommend topical gels, or suggest physical therapy to keep you moving. For chemo-nerve pain, drugs like gabapentin or duloxetine, usually used for other kinds of nerve issues, can sometimes bring big relief. And don’t forget cold packs for mouth sores (cancer popsicles are a real thing, and they help).
- Moisturize skin religiously during and after radiation. Dryness makes burns worse. Some clinics recommend specific creams like calendula (a plant-based ointment), which several studies show cuts down on radiation burn pain.
- If mouth or throat pain rules your world, stick with blended, cold foods—nothing acidic or spicy. Many people rely on shakes or even baby food to get through the worst weeks.
- Try relaxation or distraction methods. Meditation apps, video games, podcasts—anything to give your brain a break from pain signals or post-treatment anxiety spirals.
- For chronic pain post-surgery, don’t wait too long to get help. Nerve pain can sometimes be reduced with early intervention—sometimes with non-surgical nerve blocks.
- Lastly, never be embarrassed about needing counseling or an antidepressant. Physical pain is often tangled up with worry and sadness; treating all sides lifts a bit of the burden.
People often want to know: does the pain at least mean the treatment is working? Sadly, there’s no real rhyme or reason. Some people get torture-level side effects and see their cancer shrink; others go through smooth treatments and don’t get good news. It’s random, and that randomness is part of what makes it so tough.
The silver lining? Cancer care keeps evolving, and each new breakthrough seems to focus more on helping people feel better as they fight disease. Robotic surgeries mean smaller cuts, fewer nerves hit. Immunotherapies are getting more precise, avoiding some of the off-target pain. Research published in the Annals of Oncology in 2023 showed that hospitals using standardized pain tracking and response cut rates of severe pain by almost 40%. That’s a major shift.
Nothing about this journey is “easy.” But most people who’ve gone through it say small victories—a night with less pain, a meal that doesn’t sting, a chance to laugh with someone you love—mean the world when everything else feels out of control. Understanding what to expect, being honest with your medical team, and leaning on every support you can—sometimes that’s the real difference between pure hell and something you can manage, one day at a time.





Rohan Talvani
I am a manufacturing expert with over 15 years of experience in streamlining production processes and enhancing operational efficiency. My work often takes me into the technical nitty-gritty of production, but I have a keen interest in writing about medicine in India—an intersection of tradition and modern practices that captivates me. I strive to incorporate innovative approaches in everything I do, whether in my professional role or as an author. My passion for writing about health topics stems from a strong belief in knowledge sharing and its potential to bring about positive changes.
view all postsWrite a comment