
Picture a tiny cell that just won't listen to anyone—keeps growing, crowds out the neighbors, never turns off. That's pretty much how cancer works. But here’s the thing: It doesn’t have unlimited freedom. Plenty of roadblocks get in its way, even inside your body right now. Some people think cancer cells are basically invincible, but that’s not the whole story.
Your immune system, of all things, is out there quietly searching and destroying troublemakers before they turn into something nasty. Ever heard of 'tumor suppressor genes'? These guys act like strict referees, blowing the whistle when a cell breaks the rules. But sometimes cancer finds creative ways to dodge or turn off these defenses.
The good news? Scientists are figuring out where the weak spots are and coming up with ways to stop cancer in its tracks. Today, your doctor can prescribe medicines that act like barricades, cutting off the fuel cancer needs to grow. There’s even research showing simple habits like regular exercise and eating more veggies might play a behind-the-scenes role in slowing things down.
- Why Do Cancer Cells Grow So Aggressively?
- The Body’s Natural Defenses Against Cancer
- Targeted Treatments: Shutting Down Growth Pathways
- Lifestyle Tweaks That Actually Make a Difference
- Immunotherapy: Letting the Body Fight Back
- New Frontiers: What’s Coming Next?
Why Do Cancer Cells Grow So Aggressively?
Here’s the blunt truth: cancer cells just don’t play by the rules. Normal cells know when to stop dividing. They get old, damaged, or crowded and simply call it quits. Cancer cells totally ignore those signals. They keep multiplying, even when they shouldn’t, and don’t die off like healthy cells do. That’s a big part of what makes cancer growth such a headache.
What’s driving this out-of-control behavior? It usually boils down to broken or mutated genes. Picture an old light switch that’s stuck in the "on" position—cancer genes can lock a cell into nonstop division. Tumor suppressor genes (like the famous p53) are supposed to slow things down, but if they’re damaged or switched off, the brakes just don’t work. At the same time, other genes called oncogenes push cells to start multiplying like crazy.
Another sneaky trick: cancer cells can hijack the body’s supply lines. They actually send out signals that help grow new blood vessels (the process is called angiogenesis), pulling in the nutrients and oxygen cancer needs to keep expanding. Some types of cancer can even dodge the body’s death-program for sick cells—a process called apoptosis—letting damaged, dangerous cells stick around.
To put numbers to it, certain types of cancer double the number of cells in just a few weeks. For example, fast-growing cancers like leukemia or some lung cancers can go from a cluster of cells to a noticeable tumor in months.
| Cancer Type | Average Doubling Time |
|---|---|
| Lung cancer | 3-6 months |
| Leukemia | 2-4 weeks |
| Breast cancer | 2-3 months |
This growth means that catching cancer cells early matters—a lot. Not all tumors are this fast, but the ones that are, need quick and aggressive strategies for cancer treatment. That’s why understanding what makes these cells tick is a huge focus in medical research right now. It’s the first step to shutting them down.
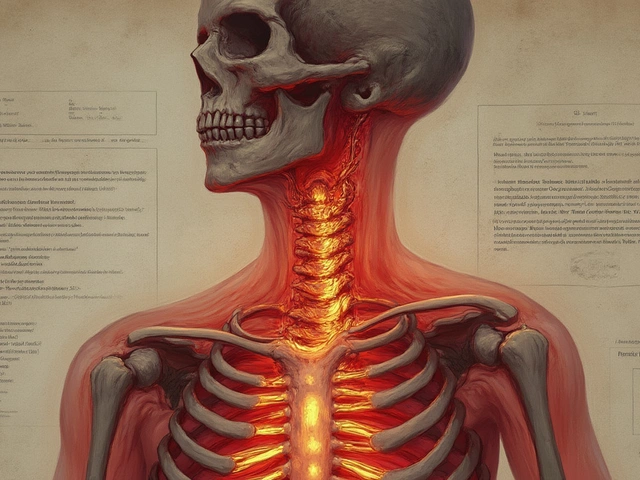
The Body’s Natural Defenses Against Cancer
You might not realize it, but your body fights off cancer growth every single day. Your immune system isn’t just there to take down colds or flus. It's also on constant patrol for cells that could turn into cancer cells.
The most important players here are white blood cells. Think of them as security guards. Some, like T-cells and natural killer cells, hunt down weird or damaged cells and tell them, “Get out.” When they spot a cell acting up—maybe dividing out of control—they can zap it before things get ugly.
Another key defense: Tumor suppressor genes. Genes like p53 and RB act like the brakes on a bike. They tell cells when to stop multiplying or repair themselves. If these genes catch a problem, they can even order a cell to self-destruct before it causes trouble. Let’s break it down:
- p53 gene: Checks cell DNA and decides if the cell is safe. If not, it directs the cell to die off, which stops faulty cells from turning cancerous.
- RB gene: Keeps cells from dividing too fast. If it spots an issue, it slams on the brakes.
- Immune surveillance: Your immune system performs regular “security sweeps,” removing cells that look suspicious.
You might be surprised—researchers found that people with weakened immune systems (like transplant patients) are several times more likely to get cancer. That says something big about just how busy your internal security team really is.
| Defense | Main Job | What Happens if It Fails? |
|---|---|---|
| White Blood Cells | Patrol and destroy odd cells | Possible growth of tumor |
| p53 gene | Checks DNA; orders cell suicide if needed | Damaged cells multiply |
| RB gene | Stops uncontrolled cell division | Cells divide too quickly |
Strong natural defenses don't guarantee you’ll never get cancer, but they slow things down—a lot. Doing your bit to support them (like getting enough sleep and cutting back on stress) can really help your body keep problem cells in check.
Targeted Treatments: Shutting Down Growth Pathways
Back in the day, cancer treatment meant blasting anything that divides quickly. That’s why people lost their hair during chemo—it hit healthy and cancer cells alike. Nowadays, targeted treatments have totally changed the game. Doctors can now send drugs straight at the parts of a cancer cell that help it grow, almost like flipping off a light switch only cancer uses.
Here’s how it works: cancer cells often rely on certain "growth pathways"—basically, signals inside the cell that tell it to keep dividing. When researchers figure out which signal is broken or stuck in the "on" position, drug companies make treatments to block it. For example, some breast cancers have way too much HER2 protein. There’s a drug, trastuzumab (you might know it as Herceptin), that targets that exact protein and slows the cancer down.
There are actually several types of targeted treatment:
- Monoclonal antibodies: These attach to specific proteins on cancer cells—think of them as a "wanted" poster tagging the bad guys so your immune system can find them.
- Kinase inhibitors: These block enzymes (called kinases) which cancer cells use like an accelerator pedal for growth. Imatinib (Gleevec) is famous for shutting down chronic myeloid leukemia this way.
- Angiogenesis inhibitors: These stop tumors from building new blood vessels, cutting off their food supply. Bevacizumab (Avastin) is one example.
Check out this simple comparison table:
| Treatment Type | How It Works | Common Example |
|---|---|---|
| Monoclonal antibody | Flags cancer cells for immune attack | Rituximab (Rituxan) |
| Kinase inhibitor | Blocks growth signals inside cancer | Imatinib (Gleevec) |
| Angiogenesis inhibitor | Stops blood vessels from feeding tumor | Bevacizumab (Avastin) |
The cool part? These drugs can go after the busted wiring inside a cancer cell without wrecking healthy ones nearby. Of course, they don’t work for everyone or every cancer, mainly because not all tumors rely on the same pathways. A study published in the New England Journal of Medicine showed that people with lung cancers carrying a certain EGFR mutation who took an EGFR inhibitor actually lived twice as long without their tumor getting worse, compared to those on regular chemo. That’s not a small upgrade.
"Targeted therapies have ushered in a new era in cancer management, providing options that often mean less toxicity and better quality of life," says Dr. Charles Sawyers, a major name in cancer research.
It’s not perfect—sometimes the cancer mutates again and dodges the drug, and side effects can still show up. But this approach lets your doctor match the right tool to the right job, which was just a dream a couple of decades ago. Ask your doctor if your tumor has these "targetable" markers. You’d be surprised how often technology can make a difference in shutting down those cancer growth engines.

Lifestyle Tweaks That Actually Make a Difference
Most people don’t realize how much daily habits can put the brakes on cancer growth. There’s no magic meal or silver bullet, but changing a few things in your routine can help your body’s defenses do their job. Real-world studies keep pointing to a simple truth: tiny choices stack up over time.
Let’s talk food first. You don’t have to swear off pizza, but eating more fruits, veggies, and whole grains actually helps tamp down inflammation. Cells love it when they’re not drowning in processed foods and sugar. Broccoli, berries, spinach, and beans—these foods aren’t just ‘good for you’ in theory; they have chemicals that slow down cancer cell growth in the lab.
- Move your body every day. You don’t have to run marathons. Even brisk walking or cycling for 30 minutes can lower the risk of new or returning tumors by around 20% in some types of cancer.
- Keep weight in check. Fat tissue produces hormones that can mess with normal cell signals. Just losing as little as 5% of your body weight can shift things in your favor.
- Don’t light up. This isn’t news, but worth repeating: stopping smoking drops cancer risk way faster than most expect. Within five years of quitting, lung and mouth tumor risks drop noticeably.
- Cut back on alcohol. Anything above a drink a day—even red wine—nudges the odds the wrong way for many cancers.
Here’s a quick look at what the stats say:
| Lifestyle Tweak | Possible Reduction in Cancer Risk |
|---|---|
| Exercise 150 minutes/week | Up to 25% for colon and breast cancers |
| Eat 5+ servings of fruit/veg daily | About 10% lower risk across cancer types |
| Quitting smoking | 40-70% drop for lung, mouth, throat cancers in 5 years |
None of this is a replacement for treatment, but don’t underestimate these lifestyle moves. My wife, Anjali, nudged me into swapping sugary snacks for nuts, and it’s honestly way easier to keep the habit than I thought. Pick one mountain at a time—small steps really do help put the squeeze on those annoying cancer cells.
Immunotherapy: Letting the Body Fight Back
For a long time, nobody thought the immune system could take on cancer. Turns out, it just needed help spotting the sneaky bad guys. That’s where immunotherapy comes in. It basically gives your immune cells the boost they need to find and kill cancer, instead of letting those cells blend in.
The trick is, cancer cells put up a kind of ‘don’t attack me’ shield. You might hear doctors talk about “checkpoint inhibitors”—these drugs remove that shield so your body’s natural defense team (like T-cells) can get to work. The drugs pembrolizumab and nivolumab are two checkpoint inhibitors used for things like melanoma, lung cancer, and head and neck cancers. There’s real proof these treatments can shrink tumors or even hold them steady for years.
- CAR-T cell therapy: Doctors take some of your immune cells, beef them up in a lab, and put them back in you, supercharged to hunt down cancer.
- Cytokine therapy: These treatments amp up the immune system with extra signaling proteins, making sure the anti-cancer army gets the message.
Immunotherapy isn’t a magic bullet. It works best for certain types of cancer but isn’t for everyone. Side effects can pop up—sometimes the immune system goes after healthy cells, causing inflammation in places like the gut, skin, or lungs. But lots of people get back years of life after treatments like these, with fewer of the harsh side effects you see in regular chemo.
| Type of Immunotherapy | Main Cancers Treated |
|---|---|
| Checkpoint Inhibitors | Melanoma, lung, bladder, kidney |
| CAR-T Cell Therapy | Leukemia, lymphoma |
| Cytokine Therapy | Kidney, melanoma |
Treatments are moving fast. New drugs come out almost every year, and doctors keep finding ways to make the immune system smarter. Ask your doctor if your type of cancer has immunotherapy options—there may be new trials worth checking out.
New Frontiers: What’s Coming Next?
The fight to stop cancer growth is moving fast. A few years ago, the idea of using your own immune system to wipe out cancer was pretty wild. Now, CAR-T cell therapy actually does just that—doctors take your immune cells, turbocharge them in a lab, and send them back into battle. For some types of blood cancer, the results have shocked everyone, with complete remissions at rates no one thought possible ten years back.
Gene editing is another game-changer. CRISPR techniques let scientists snip out broken bits of DNA that make normal cells turn cancerous. It’s early days for treating most cancers this way, but there's already a small lymphoma trial showing people staying cancer-free for months after a single treatment.
There’s also buzz about using viruses—not harmful ones, but custom-designed ones—to infect and kill cancer cells without touching healthy tissue. It's called oncolytic virus therapy. The cool part? Some of these viruses can wake up the immune system inside the tumor and make immune drugs work better.
- Liquid biopsies: Blood tests finding cancer DNA before you feel a single symptom. Catch it earlier, start treatment sooner.
- Microbiome tweaks: Gut bacteria might change how well your body blocks tumor growth. We're only starting to see how diets or probiotics might be used in cancer treatment.
- Smart drugs: Medicines that only switch on inside tumor cells, leaving healthy areas alone. Fewer side effects, better results.
Here’s a snapshot of ongoing breakthroughs:
| Frontier | Status | Where it works best (so far) |
|---|---|---|
| CAR-T Cell Therapy | Approved for some cancers | Blood cancers (like leukemia, lymphoma) |
| CRISPR Gene Editing | Early human trials | Certain inherited cancers, blood cancers |
| Oncolytic Virus Therapy | FDA-approved for melanoma | Melanoma, brain, and liver cancers (trials ongoing) |
| Liquid Biopsies | Clinical use growing | Early detection, almost all major cancers |
All this is making it tougher for cancer cells to grow unchecked. While every person’s case is different, these breakthroughs mean the next decade could look very different for anyone worried about cancer.




Rohan Talvani
I am a manufacturing expert with over 15 years of experience in streamlining production processes and enhancing operational efficiency. My work often takes me into the technical nitty-gritty of production, but I have a keen interest in writing about medicine in India—an intersection of tradition and modern practices that captivates me. I strive to incorporate innovative approaches in everything I do, whether in my professional role or as an author. My passion for writing about health topics stems from a strong belief in knowledge sharing and its potential to bring about positive changes.
view all postsWrite a comment