
Day 3 Heart Surgery Symptom Checker
Check Your Symptoms
Select any symptoms you're experiencing on your third day after heart surgery. This tool helps you distinguish normal recovery signs from warning signs that require medical attention.
Quick Takeaways
- Day 3 marks the peak of inflammation, pain, and fluid shifts after cardiac surgery.
- Common warning signs include fever, increased chest pain, rapid heartbeat, and shortness of breath.
- Effective pain control, gentle mobilization, and breathing exercises can smooth the third‑day slump.
- Call your surgical team immediately if you notice signs of infection, bleeding, or arrhythmia.
- Understanding what’s normal versus abnormal empowers you to participate actively in your recovery.
What Happens on Day 3 After Heart Surgery?
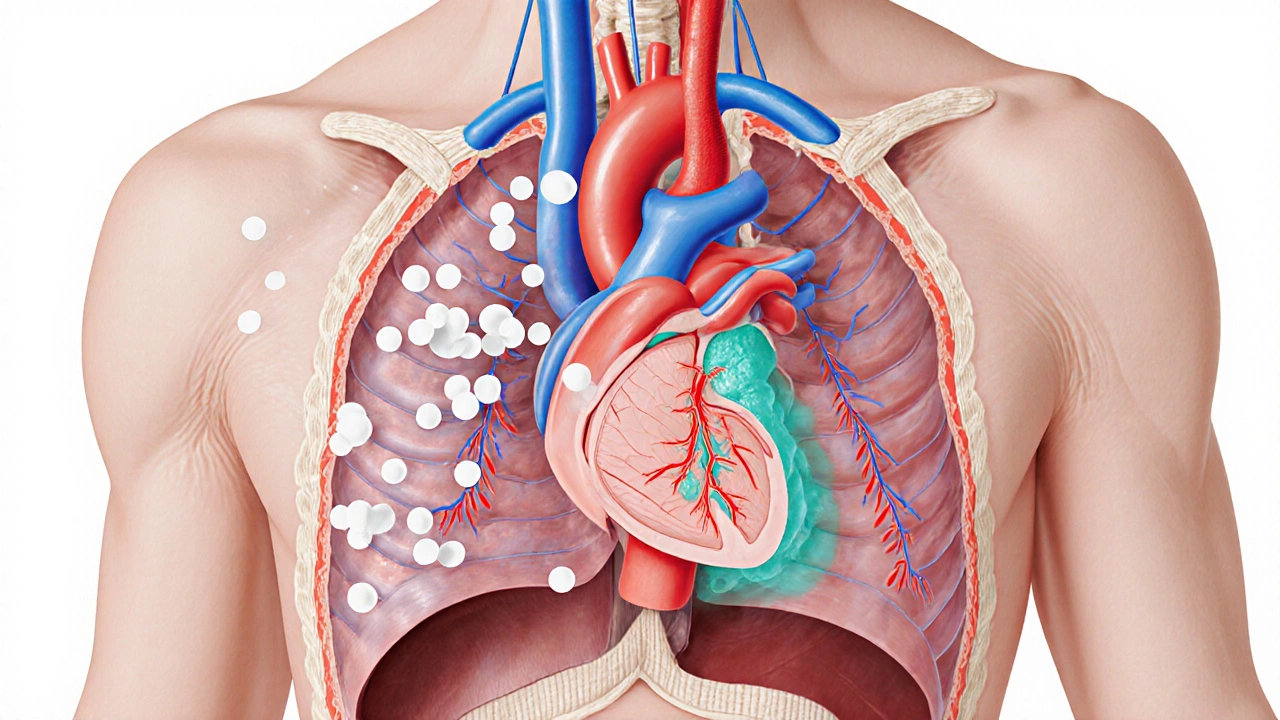
By the third postoperative day the body is still adjusting to the trauma of opening the chest, connecting a heart‑lung machine, and rerouting blood flow. Most patients are still on the intensive care unit (ICU) or a step‑down unit, hooked up to monitors that track heart rhythm, blood pressure, and oxygen levels.
Cardiothoracic surgery is a specialty that deals with procedures on the heart, lungs, and great vessels. After the operation, the body initiates a cascade of inflammatory responses that manifest as swelling, fluid buildup, and heightened pain sensitivity.
The typical timeline looks like this:
- Day 0‑1: Patient is intubated, on mechanical ventilation, and receiving high‑dose pain meds.
- Day 2: Extubation often occurs, and nurses start gentle breathing exercises.
- Day 3: Inflammation peaks, pain spikes, and the first signs of complications may appear.
Because the sternal bone is wired together, every breath or cough creates a tug on the incision site, which is why many describe day 3 as the “worst” day.
Why Day 3 Feels the Worst: Physiological Reasons
The third day coincides with three major physiological processes:
- Inflammatory response peaks as white blood cells flood the chest cavity, releasing cytokines that cause swelling and pain.
- Fluid shifts lead to pericardial effusion, a small collection of fluid around the heart that can make the pulse feel racing.
- Recovery of cardiac rhythm may be uneven, resulting in occasional arrhythmia (irregular heartbeat) as the heart’s electrical system recalibrates.
These three factors amplify pain, fatigue, and the sensation of “something’s not right.” Additionally, patients often taper off opioid painkillers around day 3, exposing a temporary gap in pain coverage.
Common Complications to Watch For
While most patients glide through day 3 without serious issues, a handful of complications tend to surface at this stage. Knowing the red flags helps you act quickly.
| Normal Recovery Sign | Potential Warning Sign |
|---|---|
| Mild chest discomfort that eases with shallow breathing | Sharp, worsening pain that radiates to the back or jaw |
| Low‑grade fever (under 100.4°F / 38°C) | Fever above 101°F (38.5°C) with chills |
| Heart rate 70‑90 bpm, regular rhythm | Rapid heartbeat (>110 bpm), irregular rhythm, palpitations |
| Shortness of breath that improves with sitting up | Persistent dyspnea, coughing up pink frothy sputum |
| Incision site with slight swelling and minimal drainage | Increasing redness, warmth, or pus-possible sternal wound infection |
Other complications that may emerge on day 3 include:
- Pulmonary embolism: a blood clot that travels to the lungs, causing sudden chest pain and severe shortness of breath.
- Anemia from postoperative blood loss, leading to fatigue and light‑headedness.
- Graft dysfunction (in bypass surgery) showing as low output or new murmurs.
Managing Pain and Discomfort
Effective pain control on day 3 is a balancing act between keeping you comfortable and avoiding over‑sedation.
- Scheduled non‑opioid meds: Acetaminophen and ibuprofen (if not contraindicated) are given every 6 hours to blunt the inflammatory pain.
- Patient‑controlled analgesia (PCA): If you still have a PCA pump, adjust the dose as instructed by the nurse. Use the button sparingly-each dose is typically low‑dose morphine.
- Regional blocks: Some centers place a continuous epidural or intercostal catheter that delivers local anesthetic directly to the chest wall.
- Ice packs: Applying a thin ice pack (wrapped in a towel) to the sternum for 15‑minute intervals can numb superficial pain.
Combine medication with non‑pharmacologic methods: deep breathing, guided relaxation, and gentle coughing exercises (with a splint or pillow to protect the incision).

Tips for a Smoother Recovery on Day 3
- Stay hydrated: Small sips of water every 30 minutes keep mucus thin and support kidney function.
- Early ambulation: Even a two‑minute walk in the hallway, with a nurse’s assistance, reduces clot risk and improves lung expansion.
- Incentive spirometry: Take 10 deep breaths every hour; this inflates the lungs and prevents atelectasis.
- Nutrition: Aim for protein‑rich foods (Greek yogurt, eggs, lean meat) to aid tissue healing.
- Sleep hygiene: Keep the room dim, use earplugs, and request a low‑dose nighttime analgesic to break up the pain‑wake‑pain cycle.
- Monitoring: Keep a diary of pain scores, temperature, and any new symptoms. Share it with the care team during rounds.
When to Call Your Surgeon or Emergency Services
Most concerns can be raised with the bedside nurse, but certain signs require immediate action:
- Chest pain that feels crushing, lasts more than a few minutes, or spreads to the arm or jaw.
- Sudden, severe shortness of breath or a feeling of suffocation.
- Fever above 101°F (38.5°C) with chills, especially if accompanied by wound drainage.
- Rapid heartbeat (>130 bpm) that does not settle with rest.
- Bleeding that soaks more than one dressing in an hour or bright red blood spurting from the incision.
If any of these occur, call the cardiac unit directly or dial emergency services. Prompt treatment can prevent a minor issue from becoming life‑threatening.
Frequently Asked Questions
Why does the incision hurt more on day 3 than on day 1?
Incision pain follows a U‑shaped curve. The first 24 hours are covered by high‑dose opioids, which mask the true intensity. By day 3, the medications taper and the inflammatory cascade peaks, making the pain feel louder.
Is it normal to feel shortness of breath when I cough?
A mild, brief shortness of breath is expected because the chest wall is still stiff. However, persistent wheezing, pink frothy sputum, or a sudden drop in oxygen saturation signals a problem and should be reported.
Can I walk on my own on day 3?
Most hospitals encourage a short, assisted walk as early as the second day. By day 3 you should be able to take a few steps with a nurse or physical therapist, but avoid long distances until cleared.
What does a low‑grade fever mean?
A temperature under 100.4°F (38°C) is usually part of the normal inflammatory response. If the fever climbs higher or lasts more than 48 hours, infection becomes more likely.
Should I use heating pads on my sternum?
Heat can increase swelling and is not recommended for the first two weeks. Stick to cold therapy (brief ice packs) and follow the surgeon’s wound‑care instructions.
Understanding the why behind day 3’s discomfort empowers you to manage it effectively. With the right meds, breathing exercises, and vigilance for warning signs, you’ll move past the rough patch and keep healing toward a stronger heart.





Rohan Talvani
I am a manufacturing expert with over 15 years of experience in streamlining production processes and enhancing operational efficiency. My work often takes me into the technical nitty-gritty of production, but I have a keen interest in writing about medicine in India—an intersection of tradition and modern practices that captivates me. I strive to incorporate innovative approaches in everything I do, whether in my professional role or as an author. My passion for writing about health topics stems from a strong belief in knowledge sharing and its potential to bring about positive changes.
view all postsWrite a comment