
Recovery Timeline Calculator
Personalized Recovery Estimate
Enter your details to get an estimated recovery timeline based on medical best practices.
Your Recovery Timeline
Standard Protocol
Estimated completion time:
Accelerated Protocol
Estimated completion time:
Key Milestones
Your Personal Recommendations
Quick Takeaways
- Start gentle range‑of‑motion exercises within the first 24‑48 hours.
- Use a balanced mix of ice, compression, and elevation to control swelling.
- Schedule daily sessions with a physiotherapist for the first 2‑3 weeks.
- Prioritise protein‑rich foods, hydration, and good sleep to speed tissue repair.
- Watch for warning signs like increasing pain, redness, or unexplained fever.
When you walk out of the operating theatre, the real work begins. Knee replacement recovery refers to the period after total knee arthroplasty when the joint heals and you regain function can feel daunting, but the right plan can shave weeks off the usual timeline. Below is a step‑by‑step guide that combines medical best‑practice with practical tips you can start today.
Understanding the Healing Timeline
Most surgeons expect a baseline of 6‑12 weeks before you feel steady on your feet. knee replacement recovery isn’t a one‑size‑fits‑all process; age, pre‑op fitness, and the surgical technique all play a role. Knowing what’s “normal” helps you spot genuine setbacks early.
Day‑by‑Day Post‑Op Checklist
- Day 0‑1 (Hospital Stay): Begin ankle pumps and quadriceps sets under nurse supervision. Keep the leg elevated above heart level when you’re sitting or lying down.
- Day 2‑3: Start gentle passive knee flexion using a continuous passive motion (CPM) machine if your surgeon recommends it. Begin short, assisted walks with a walker or crutches.
- Day 4‑7: Transition to a cane, increase walking distance by 5‑10 minutes per day, and add active straight‑leg raises.
- Week 2‑3: Begin supervised Physical therapy structured sessions that focus on range of motion, strength, and gait training. Aim for at least three 45‑minute appointments.
- Week 4‑6: Introduce low‑impact cardio (stationary bike or pool walking). Start closed‑chain exercises like mini‑squats.
- Week 6‑12: Progress to functional activities-stairs, light jogging, or cycling-guided by your therapist.
Core Rehab Strategies
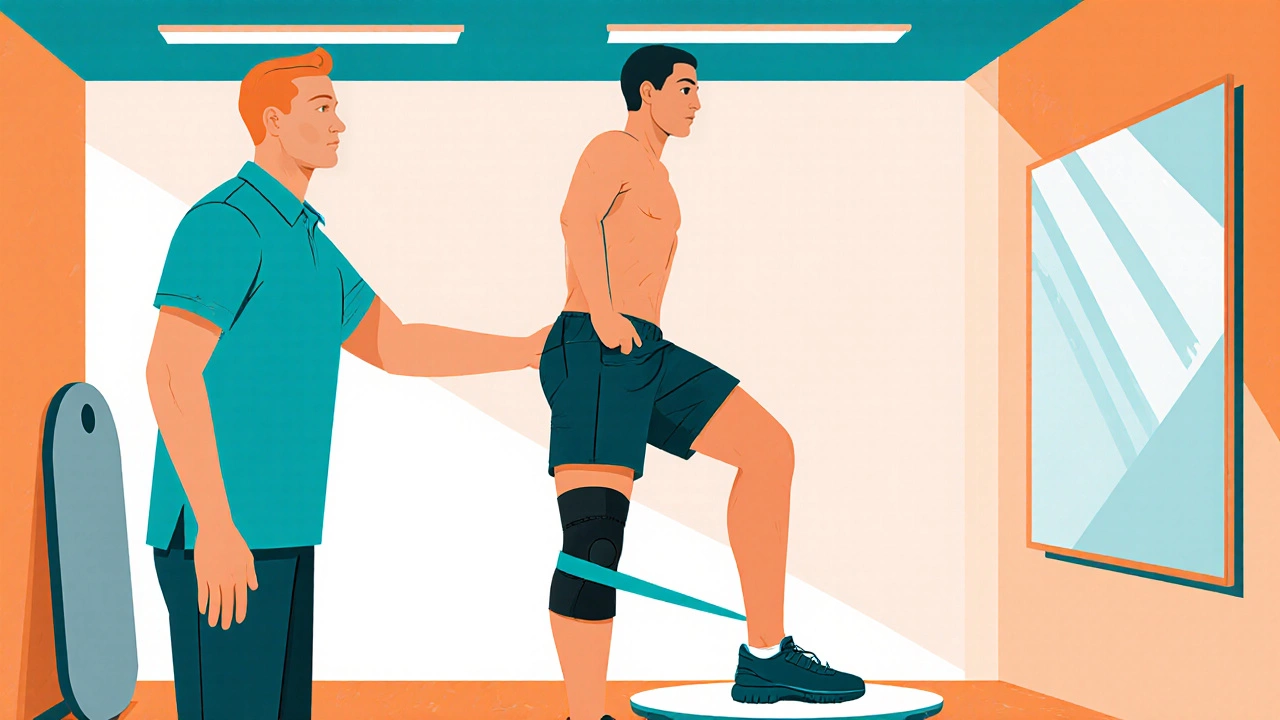
Three pillars drive a speedy recovery: mobility, strength, and proprioception.
- Range‑of‑Motion (ROM) drills: Heel slides, seated knee bends, and wall slides. Aim for 90° flexion by week 2 and 120° by week 6.
- Strength building: Quad sets, straight‑leg raises, and resistance band leg presses. Use a light band (5‑10lb) and increase resistance weekly.
- Proprioceptive work: Balance board or single‑leg stance for 30 seconds, three times a day, once you can bear weight safely.
Nutrition & Lifestyle Hacks
Your body needs fuel to knit tissue together. Here’s the eating plan that supports healing:
- Protein: 1.2‑1.5g per kilogram of body weight daily. Lean poultry, fish, Greek yogurt, and legumes are top choices.
- VitaminC & Zinc: Antioxidant and collagen support. Include citrus, bell peppers, nuts, and pumpkin seeds.
- Omega‑3 fatty acids: Reduce inflammation. Add salmon, walnuts, or a fish‑oil supplement.
- Hydration: Aim for 2‑3L of water a day to keep synovial fluid lubricated.
- Sleep: 7‑9hours of quality rest accelerates protein synthesis and hormonal recovery.
Managing Pain & Swelling
Effective pain control lets you move, and movement reduces swelling-a virtuous cycle.
- Ice therapy application of cold packs for 15‑20 minutes every 2‑3 hours during the first 72hours.
- Compression garments elastic sleeves that apply graduated pressure to limit fluid build‑up. Wear them while walking.
- Elevation keeping the leg raised above heart level to encourage venous return whenever you’re seated.
- Follow the prescribed medication schedule-usually a combination of acetaminophen, NSAIDs, and, if needed, short‑term opioids.
Reducing Complications
Complications like blood clots or infection can set you back months.
- Blood clot prevention use of low‑molecular‑weight heparin or direct oral anticoagulants as ordered by your surgeon plus ankle pumps every hour while awake.
- Maintain wound hygiene-clean with saline, keep the dressing dry, and report any increasing redness or drainage.
- Start gentle walking as soon as the surgeon allows; movement is the single best defense against deep‑vein thrombosis.

When to Push Harder vs. Rest
Listening to your body matters. Use these signals:
- Green light: Mild soreness that eases after a short rest, steady improvement in ROM, no swelling beyond 24hours.
- Yellow light: Sharp pain that spikes during a specific movement, swelling that persists >48hours, mild fever (<38°C).
- Red light: Intense, localized pain, rapidly increasing swelling, fever >38°C, or wound drainage-stop activity and call your surgeon.
Comparison of Standard vs. Accelerated Rehab Protocols
| Milestone | Standard Protocol | Accelerated Protocol |
|---|---|---|
| First unassisted walk | Days 3‑5 | Day 2 |
| Full extension (0°) | Week 2 | Day 7‑10 |
| 90° flexion | Week 4 | Week 2 |
| Stair climbing without aid | Week 6‑8 | Week 4 |
| Return to light jogging | Month 4‑6 | Month 3 |
Both pathways aim for safe healing; the accelerated track leans heavily on early mobilization, aggressive pain control, and daily therapist visits. Choose the one that matches your health status and surgeon’s advice.
Next Steps & Troubleshooting
If you hit a plateau-say, stuck at 70° flexion after week 3-try these quick fixes:
- Re‑evaluate pain meds; uncontrolled pain limits effort.
- Add a warm‑up before stretching (e.g., a short heat pack for 5minutes).
- Check your shoe wear; unsupportive footwear can hinder gait training.
- Ask your therapist to incorporate manual therapy (soft‑tissue mobilization) once a week.
Always keep open communication with your surgeon and physiotherapist. A minor tweak early on can prevent a major delay later.
Frequently Asked Questions
How soon can I drive after a knee replacement?
Most patients regain enough strength to drive safely after 4‑6 weeks, provided they can operate the pedals without pain and have a full‑leg extension. Always get clearance from your surgeon.
Is it safe to use a stationary bike during the first month?
Yes, a low‑resistance bike helps improve range of motion and circulation without loading the joint. Start with 5‑10 minutes and gradually increase as tolerated.
What are red‑flag signs of infection?
Increasing redness, warmth, swelling, foul‑smelling drainage, or a fever above 38°C are warning signs. Contact your surgical team immediately.
Can I take a shower instead of a full bath?
A gentle shower is fine after the first 24‑48hours, as long as you keep the incision dry. Use a handheld showerhead and avoid high‑pressure streams directly on the wound.
When is it okay to stop using crutches?
Typically after 2‑3 weeks, once you can walk 20‑30minutes without pain or instability and have good balance on a single cane.





Rohan Talvani
I am a manufacturing expert with over 15 years of experience in streamlining production processes and enhancing operational efficiency. My work often takes me into the technical nitty-gritty of production, but I have a keen interest in writing about medicine in India—an intersection of tradition and modern practices that captivates me. I strive to incorporate innovative approaches in everything I do, whether in my professional role or as an author. My passion for writing about health topics stems from a strong belief in knowledge sharing and its potential to bring about positive changes.
view all postsWrite a comment